According to GLOBOCAN 2022, thyroid cancer is one of the most common malignancies worldwide, with approximately 16,800 new cases and 8,400 deaths recorded. In Vietnam, this disease ranks 6th among the 10 most common cancers, with 6,122 new cases and 858 deaths reported annually.
The thyroid is an endocrine gland located at the front of the neck. It produces essential hormones such as Thyroxine (T4) and Triiodothyronine (T3), which regulate and control the body’s metabolic processes. Thyroid cancer not only affects hormone production but also disrupts metabolic functions, leading to serious health complications.
1. WHAT IS THYROID CANCER?
Thyroid cancer occurs when thyroid cells become abnormal and transform into malignant cells, forming tumors within the gland. Although the mortality rate of this cancer is relatively low compared with many other malignancies, if not diagnosed and treated promptly, the cancer cells can spread beyond the thyroid, invading nearby lymph nodes in the neck or metastasizing to other organs. This can cause severe damage, impair body functions, and ultimately threaten the patient’s life.

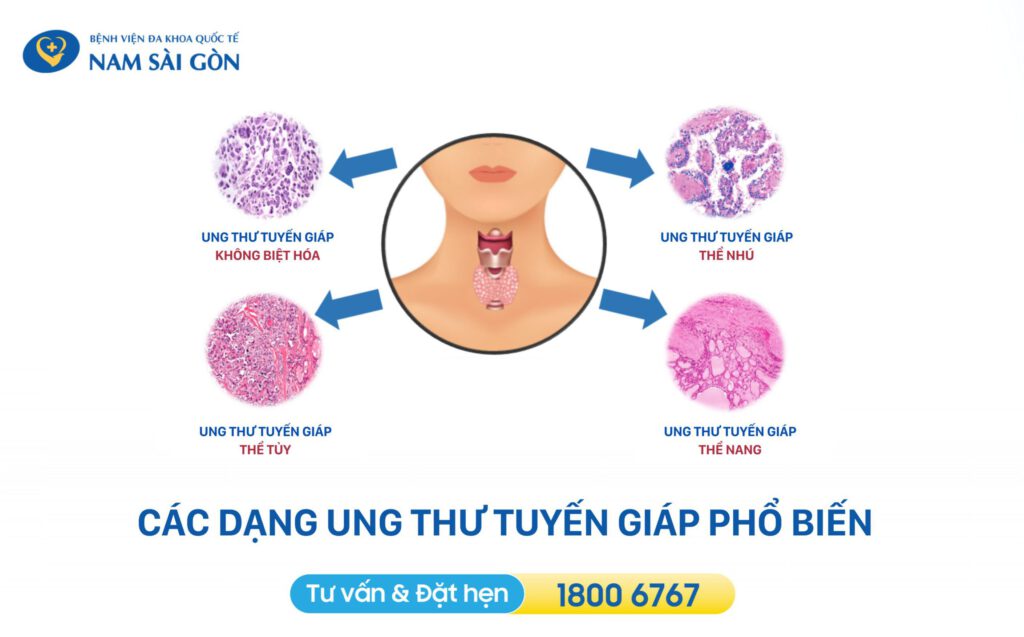
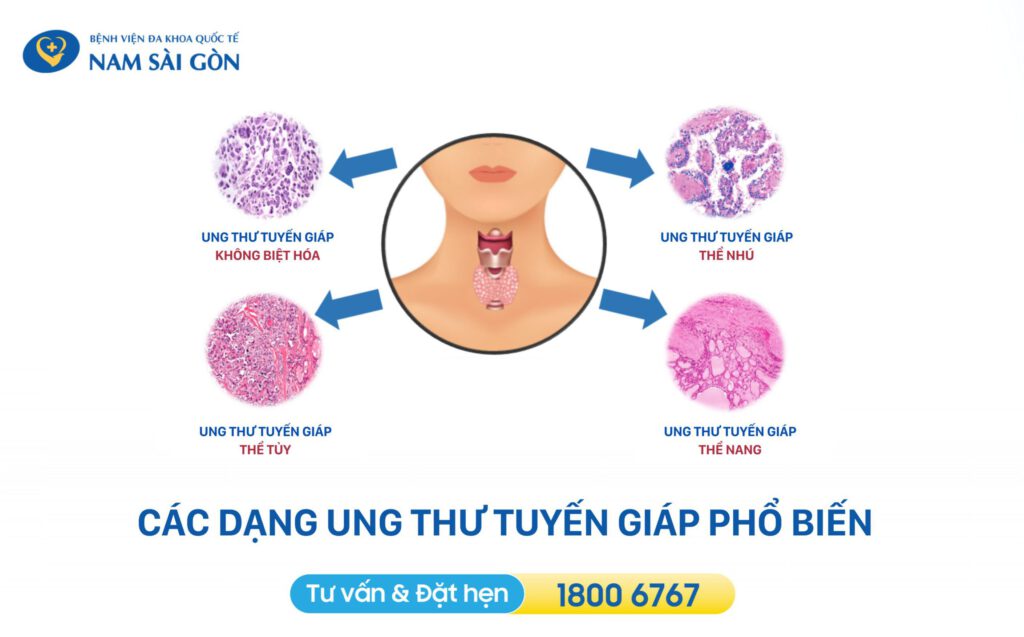
2. Classification of thyroid cancer
Based on cytological characteristics and the degree of malignancy, thyroid cancer is classified into two major categories: differentiated thyroid cancer and undifferentiated thyroid cancer.
Differentiated Thyroid Cancer (DTC)
Differentiated thyroid cancer refers to cases in which cancer cells still retain some structural and functional features of normal thyroid cells. This is the most common form, accounting for 80%–90% of all thyroid cancer cases. The disease usually progresses slowly and often causes no obvious symptoms, as the tumors are typically small, mobile, and painless when touched. However, they can be easily detected through routine thyroid ultrasound, and they respond well to early treatment.
Differentiated thyroid cancer includes three main types:
-
Papillary Thyroid Carcinoma (PTC)
This is the most common type, accounting for about 80% of cases. It usually grows slowly and rarely causes death when detected early and treated appropriately.
-
Follicular Thyroid Carcinoma (FTC)
Originating from thyroid follicular cells, this type accounts for about 10% of cases. Compared with papillary carcinoma, follicular carcinoma is more aggressive because it can spread beyond the thyroid gland. Despite this, it can still be treated effectively if detected early.
-
Medullary Thyroid Carcinoma (MTC)
Although classified as a differentiated cancer, medullary carcinoma has distinct features. It arises from parafollicular (C) cells, which produce calcitonin, a hormone responsible for regulating calcium levels in the blood.
Undifferentiated (Anaplastic) Thyroid Cancer
Undifferentiated or anaplastic thyroid cancer occurs when cancer cells no longer retain any characteristics of normal thyroid cells. These cells divide extremely rapidly, are highly invasive, and can quickly spread to nearby structures as well as distant organs such as the bones and lungs.
Although rare, anaplastic thyroid cancer is considered the most dangerous and aggressive form of thyroid malignancy.
Clinical signs often include:
-
A large, hard thyroid mass that is difficult to move
-
Tumor invasion into surrounding tissues
-
Symptoms such as difficulty swallowing (dysphagia), changes in voice, or hoarseness
3. Signs and Symptoms of Thyroid Cancer
Thyroid cancer often presents with no obvious symptoms in its early stages, but it can be recognized through the following signs:
-
Neck lump:
The most common sign is a soft, mobile, and painless mass in the neck.
-
Voice changes:
Hoarseness or voice alterations may occur if the tumor compresses the recurrent laryngeal nerve.
-
Difficulty swallowing (dysphagia):
As the tumor enlarges, it may press against the esophagus, causing trouble swallowing or the sensation of something stuck in the throat.
-
Swollen lymph nodes:
Enlarged cervical lymph nodes, particularly common in papillary thyroid carcinoma.
-
Neck pain or discomfort:
Some patients may experience mild pain or discomfort in the neck, especially when talking or swallowing.
-
Unexplained fatigue, weight loss, frequent diarrhea, bone pain, and other systemic symptoms.
In its early stages, thyroid cancer typically lacks clear symptoms, making it easy to overlook until it progresses and clinical signs appear. By then, the chances of successful treatment may decrease. Therefore, regular thyroid cancer screening is essential for early detection and timely management.

4. Causes of Thyroid Cancer
The exact cause of thyroid cancer remains unclear. However, several factors are known to increase the risk of developing the disease:
Exposure to ionizing radiation—such as undergoing radiation therapy—significantly increases the risk of thyroid cancer.
Statistics show that more than 70% of thyroid cancer patients have a family history of the disease. Hereditary thyroid cancers account for an estimated 5–10% of all cases.
Women—especially middle-aged and older women—are at higher risk.
Frequent alcohol consumption, smoking, and being overweight or obese contribute to a higher likelihood of developing thyroid cancer.
- Existing thyroid disorders
Conditions such as hyperthyroidism, hypothyroidism, and other thyroid-related syndromes may increase the risk.
5. High-Risk Groups for Thyroid Cancer
Certain groups of people are at higher risk of developing thyroid cancer, including:
-
Women, who have a significantly higher incidence of thyroid cancer than men — especially middle-aged and older women.
-
Individuals with a family history of thyroid cancer.
-
People who have been exposed to radiation.
-
Those with endocrine disorders.
-
Individuals living in areas with radioactive contamination.
-
People with a diet low in iodine.

6. Complications of Thyroid Cancer
Thyroid cancer—especially the undifferentiated (anaplastic) type—is a dangerous malignancy. If not detected early, it can lead to severe complications that negatively impact health and may threaten the patient’s life. Some complications that may occur in advanced stages or even after treatment include:
- Spread to lymph nodes and other organs
Cancer cells can spread from the thyroid to nearby lymph nodes in the neck, or further to organs such as the lungs, bones, and liver.
- Thyroid hormone imbalance
Cancerous cells can damage the thyroid gland, causing hormone imbalance and leading to metabolic disorders and other health problems.
- Voice changes or difficulty swallowing
These occur due to damage or compression of the recurrent laryngeal nerve.
Although early treatment significantly improves outcomes, thyroid cancer may still recur in some patients.
7. Diagnosis of Thyroid Cancer
Diagnosing thyroid cancer is a crucial step that helps determine the cancer type and stage, enabling physicians to choose the most appropriate treatment approach. The diagnostic process typically includes the following steps:
Clinical Evaluation
- Neck examination:
Assessment of the size, shape, and mobility of the thyroid gland to identify any potential masses.
- Medical and family history:
Review of symptoms, history of radiation exposure, family history of thyroid cancer, and other endocrine disorders.
Diagnostic Tests
- Thyroid ultrasound:
A widely used, non-invasive imaging method that evaluates the structure of the thyroid and detects small nodules. Ultrasound also helps guide further diagnostic procedures.
- Blood tests:
Measurement of thyroid hormone levels (TSH, T3, T4) and other markers to assess thyroid function.
- Fine-needle aspiration (FNA):
A minimally invasive procedure in which a small needle is used to obtain a sample of thyroid tissue. The sample is examined under a microscope to determine whether the nodule is benign or malignant.
- CT scan or MRI:
Used to assess the extent of tumor spread or metastasis.
- Radioactive iodine scan:
A test that evaluates thyroid function and iodine uptake, useful for identifying specific types of thyroid cancer that may not be easily detected through other methods.

8. Treatment Methods for Thyroid Cancer
Depending on the cancer type, stage of the disease, the patient’s overall health, and treatment goals, specialists will choose the most appropriate therapeutic approach. Below are some of the common treatment methods for thyroid cancer.
8.1 Thyroid Surgery

Surgical options for thyroid cancer are typically selected by specialists based on appropriate treatment goals tailored to each patient’s condition.
8.1.1 Primary Goals of Thyroid Surgery
-
Remove the thyroid lobe or the entire thyroid gland containing cancerous cells, and remove any lymph nodes suspected of metastasis.
-
Preserve thyroid endocrine function in selected cases, helping patients avoid the need for full hormone replacement therapy.
-
Protect the parathyroid glands, which regulate calcium levels in the body, thereby reducing the risk of postoperative hypocalcemia.
-
Minimize postoperative complications, such as bleeding, infection, nerve injury, or functional disorders.
-
Improve the patient’s quality of life by effectively controlling the disease with the least impact on daily activities.
8.1.2 Types of Thyroid Surgery in the Treatment of Thyroid Cancer
- Lobectomy (Removal of one thyroid lobe):
Indicated for early-stage thyroid cancer or small thyroid nodules. This procedure preserves part of the thyroid gland, allowing the body to maintain natural hormone production. However, if the tumor is not completely removed, the risk of recurrence remains high.
- Total thyroidectomy (Removal of the entire thyroid gland):
Recommended for cases of advanced or widely spread thyroid cancer, or when the risk of recurrence is high. Patients require lifelong hormone replacement therapy and may face complications such as injury to the recurrent laryngeal nerve.
- Neck lymph node dissection:
May be performed in combination with thyroid surgery when cancer cells have spread to cervical lymph nodes.
Surgical treatment for thyroid cancer was previously performed mainly through the traditional open surgery technique, which involves a classic transverse cervical incision. However, this method has certain disadvantages, as open surgery may increase the risk of intraoperative and postoperative bleeding. In addition, the large incision often affects postoperative aesthetics, especially for female patients.
Currently, endoscopic surgery for thyroid cancer has gradually replaced traditional open surgery thanks to its outstanding advantages, including leaving no visible scar, reducing the risk of bleeding during and after surgery, and minimizing temporary hoarseness following the procedure.
Nam Sai Gon International General Hospital is developing new techniques in thyroid cancer treatment, such as endoscopic surgery via the axillary route, ultrasonic scalpel thyroid surgery, and radiofrequency ablation, offering patients more surgical options. Furthermore, the hospital accepts both health insurance and medical insurance, helping patients feel more reassured when choosing treatment at the hospital.
8.2 Radioactive Iodine Therapy
This method is particularly effective for papillary thyroid carcinoma and follicular thyroid carcinoma. Radioactive iodine is absorbed by thyroid cells, including cancer cells, and emits beta radiation to destroy any remaining cancerous cells after surgery, thereby preventing recurrence. During radioactive iodine therapy, patients must follow a low-iodine diet before and after treatment to enhance the absorption and effectiveness of radioactive iodine.
8.3 Targeted Therapy (Using Tyrosine Kinase Inhibitors)
This method is used in cases where thyroid cancer does not respond to surgery or radioactive iodine therapy, especially in metastatic disease. It helps inhibit the growth and spread of cancer cells. Tyrosine kinase inhibitors may cause certain side effects; therefore, if any abnormalities occur during treatment, patients should promptly report them to their physician.

8.4 Thyroid Hormone Therapy
After thyroidectomy, patients need thyroid hormone replacement therapy to maintain metabolic function and prevent the growth of any remaining cancer cells. This therapy must be carefully adjusted based on each patient’s specific condition to ensure effectiveness and minimize side effects.
9. How to Prevent the Risk of Thyroid Cancer
Regular Health Check-ups
If you have a family history of thyroid cancer or other risk factors, you should undergo more frequent health screenings. Thyroid ultrasound is a safe, non-invasive method for early detection of small nodules, allowing timely diagnosis and treatment. In addition, cytological diagnostic tests should be performed to detect potential early risks of thyroid cancer.
Balanced Nutrition
Increase your intake of green vegetables and fruits—foods rich in vitamins A, C, and E—which help protect cells from free radicals that can damage DNA and increase cancer risk.
Supplement iodine by using iodized salt in daily meals and consuming seafood or other natural iodine-rich foods.
Limit foods high in saturated fats, such as fast food and processed foods.
Adopt and Maintain a Healthy Lifestyle
Exercise regularly to strengthen the immune system and support hormonal balance.
Manage stress, as prolonged stress can negatively affect both immunity and endocrine functions. Engage in activities that promote mental well-being such as meditation or yoga.
Avoid smoking and limit alcohol consumption, as these substances increase the risk of many types of cancer, including thyroid cancer.
If symptoms such as fatigue, unexplained weight loss, or swollen lymph nodes in the neck appear, patients should seek professional medical advice promptly for evaluation and appropriate treatment. Being proactive in diagnosis and treatment is essential to protecting your health and improving your quality of life.
Nam Sai Gon International General Hospital