Table of Contents
ToggleREMOVAL OF GIANT TUMOR “HUGGING” THE TRACHEA FOR A 75-YEAR-OLD MAN
-
Author: BỆNH VIỆN ĐA KHOA QUỐC TẾ NAM SÀI GÒN
-
19/08/2025
-
359
Updating
Just a few days’ delay could have allowed an 11-cm malignant mediastinal tumor to completely obstruct his airway. Mr. K.L, a 75-year-old patient from Cambodia, narrowly escaped death thanks to a successful partial sternotomy performed at Nam Sai Gon International General Hospital.
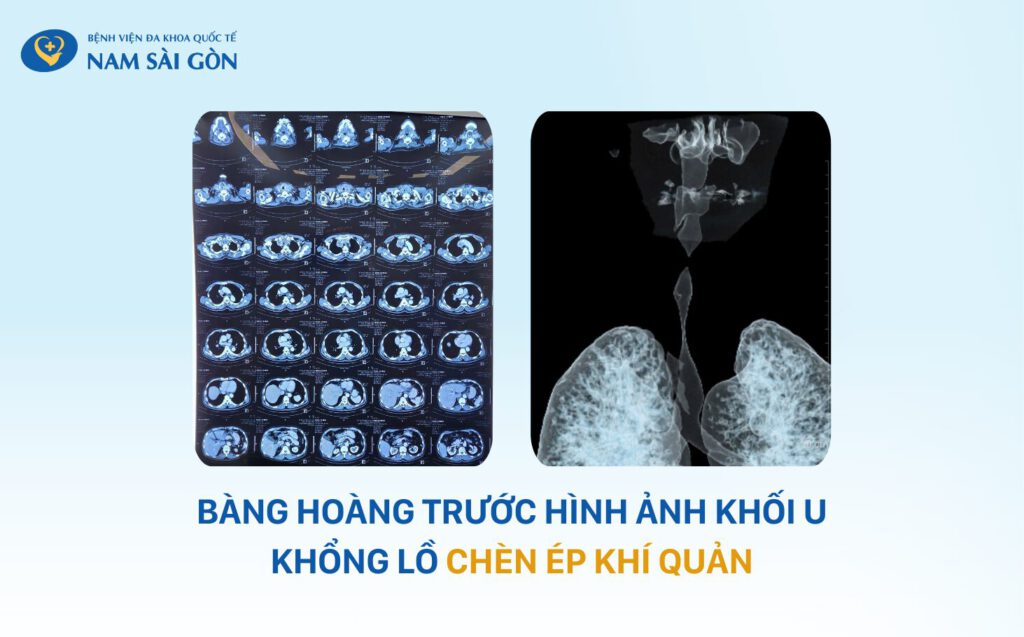
The patient shared that he had only experienced occasional shortness of breath but was otherwise able to carry on with daily activities. However, the CT scan results shocked him and his family: a massive tumor nearly 11 cm in size was extending from the neck into the chest, severely compressing the trachea, invading the entire thyroid gland, and adhering closely to major blood vessels. The narrowest portion of his trachea measured only 4.35 mm, indicating severe tracheal stenosis that made airway management extremely difficult. Imaging results also revealed multiple scattered lesions in the lungs, raising concerns that the cancer had already spread widely.
Treatment became even more challenging due to the patient’s complex underlying conditions: three-vessel coronary artery disease (with stent placement), hypothyroidism, and hypertension. Facing this critical situation, the patient sought care at Nam Sai Gon International General Hospital, hoping for a chance to survive.
Assoc. Prof. Dr. VU HUU VINH, PhD, leading thoracic surgery expert and Head of Thoracic Surgery Department at Nam Sai Gon International General Hospital, explained:
“This was an extremely complicated case. The tumor encircled, invaded, and tightly compressed the trachea, causing critical stenosis. It extended into the upper anterior mediastinum and invaded branches of the arch arteries, the innominate vein, and the superior vena cava—posing a direct threat to the patient’s life. Therefore, urgent surgery was necessary to remove the tumor and reconstruct the patient’s airway.”
A difficult decision in the consultation

This case was considered particularly challenging in terms of anesthesia and endotracheal intubation because the enlarged thyroid and mediastinal tumor were compressing the trachea. The widest part of the narrowed tracheal segment measured only 4.35 mm, whereas the endotracheal tubes commonly used for adults typically have a diameter of more than 10 mm.
Dr. Vu Thi Thu Huong (Specialist Level II) – Vice Medical Director – Head of Anesthesiology & Perioperative Care Department at Nam Sai Gon International General Hospital – explained:
“In this case, it was impossible to perform a proactive tracheostomy below the stenotic segment to maintain ventilation during anesthesia, because the narrowed area was too low and was surrounded by the tumor. Conventional endotracheal intubation was nearly impossible, and the airflow would not have been sufficient to maintain adequate oxygenation for the patient. If we could not secure the airway with an endotracheal tube, the patient could have died right on the operating table.”
Faced with this rare and highly challenging situation, with the tumor located in a “critical” position within the chest, the treatment team had to act immediately. An urgent, hospital-wide multidisciplinary consultation was convened to comprehensively evaluate treatment options and develop contingency plans for every possible scenario.
Dr. NGUYEN TRUONG KHUONG, MMed, Specialist Level II – Chief Medical Officer at Nam Sai Gon International General Hospital – shared:
“We thoroughly explained the complexity and risks of the surgery to the patient and his family. In light of their strong desire to proceed with the operation, we decided to prepare every step with the utmost care, anticipating all potential complications. Everyone gave their best effort to ensure a successful surgery and save the patient’s life.”
Three tense hours in the operating room

At 9:30 a.m., the patient was induced under endotracheal anesthesia. The surgical team—consisting of Assoc. Prof. Dr. VU HUU VINH, PhD and Dr. Pham Phu Khang (Specialist Level I), working in coordination with the anesthesiology team—began with a T-shaped incision from the neck down to the mid-chest, followed by a partial sternotomy to access the mediastinum, where the massive tumor was encasing the trachea. During surgery, part of the tumor tissue was trimmed using an ultrasonic scalpel and sent for biopsy. The results confirmed a malignant tumor.
The surgeons immediately proceeded to completely remove the mediastinal tumor along with the thyroid gland in order to preserve the major blood vessels. Hemostasis was meticulously controlled before the sternum was closed with steel wires. The entire surgery lasted three hours, yet the estimated blood loss was only approximately 450 ml—a remarkable number for a procedure of such complexity.
“It is rare for a single surgery to require three anesthesiologists. This reflects the severity of the case and the need for maximum coordination to maintain the patient’s airway. Everyone—from the surgeons to the anesthesiologists and nursing staff—put forth their best effort,” shared Dr. Pham Phu Khang, a member of the surgical team.
Speaking further about the factors contributing to the surgery’s success, Dr. Vu Thi Thu Huong (Specialist Level II) – Vice Medical Director – Head of Anesthesiology & Perioperative Care Department – noted:
“We anticipated the risks in advance and prepared multiple backup approaches. Fortunately, the remaining tracheal tissue was pliable, allowing us to use a stepwise dilation technique for intubation—starting with a very small tube of about 4.5 mm, then gradually increasing the size up to 7 mm. Thanks to this method, the team was able to secure the airway successfully and ensure the patient’s safety throughout the entire operation.”
Returning to normal life after a nerve-racking surgery

After surgery, the patient was transferred to the Department of Thoracic Surgery for monitoring without requiring additional treatment in the intensive care unit. Just a few days later, he was able to breathe deeply with ease, eat normally, and resume daily activities almost as usual. Thankfully, Mr. K.L could converse comfortably with his family without experiencing the shortness of breath he once had.

Considered an exceptionally complex and highly challenging case, the surgery required not only advanced technical expertise but also seamless coordination among multiple specialties and the support of modern medical equipment.
This success not only saved the patient’s life but also reaffirmed the hospital’s clinical capability, its proficiency in handling rare and complicated cases, and its unwavering commitment to the principle of “Everything for the patients!” at Nam Sai Gon International General Hospital.
Nam Sai Gon International General Hospital
No. 88, Street No. 8, Trung Son Residential Area, Binh Hung Commune, Ho Chi Minh City.
Hotline: 18006767
info@nih.com.vn
Last updated: 16:49 04/12/2025





