HEMORRHOIDS – SYMPTOMS, CAUSES & TREATMENT
-
Author: BỆNH VIỆN ĐA KHOA QUỐC TẾ NAM SÀI GÒN
-
01/11/2024
-
68,286
Hemorrhoids (or haemorrhoids), also known as piles, are vascular structures in the anal canal. In their normal state, they are cushions that help with stool
Even when treated surgically, hemorrhoids can still recur and lead to unpredictable complications. Therefore, early detection and treatment of hemorrhoids are extremely important.
Hemorrhoids?
Hemorrhoids (commonly known as “piles”) are the most common condition affecting the anus. Hemorrhoids occur when the veins in the anal region become excessively dilated, forming hemorrhoidal cushions. Normally, these veins are supported and held in place by connective tissues; however, over time—especially after the age of 20—these tissues may weaken, causing the veins to sag and prolapse outward.

Factors such as straining during bowel movements, prolonged sitting, pregnancy, obesity, or a low-fiber diet can worsen this condition. Currently, the exact cause of hemorrhoids has not yet been clearly identified.
Classification of Hemorrhoids
Based on their location, hemorrhoids are classified into three main types:
- Internal hemorrhoids:
Internal hemorrhoids develop due to excessive dilation of the venous plexus in the submucosal layer above the dentate line (the boundary between the anal skin and rectal mucosa). In the early stages, the hemorrhoidal cushions are small and located deep within the anal canal, so they usually cause no noticeable symptoms. Over time, however, these hemorrhoids gradually enlarge and the supporting tissues weaken. As a result, the hemorrhoidal cushions may be pushed downward and can eventually prolapse outside the anus.
Depending on the degree of prolapse, internal hemorrhoids are classified into four grades:
Grade I internal hemorrhoids:
At this stage, hemorrhoids are newly formed and usually do not cause pain. However, during bowel movements, stool may rub against the hemorrhoidal cushions, leading to rectal bleeding.
Grade II internal hemorrhoids:
The hemorrhoidal cushions begin to prolapse but are often not clearly noticeable (they may protrude slightly into the anal canal). They can prolapse during straining but retract spontaneously without the need for manual intervention.
Grade III internal hemorrhoids:
The hemorrhoidal cushions tend to become thicker and increase in size, with a rough surface and dark red color. At this stage, they frequently prolapse during bowel movements, vigorous physical activity, or coughing, and cannot retract on their own. Manual reduction is required to push them back into the rectum.
Grade IV internal hemorrhoids:
The hemorrhoidal cushions are markedly enlarged and completely prolapsed outside the anal canal, and they cannot be reduced— even with manual pressure.
 Depending on the degree of prolapse, internal hemorrhoids are classified into four grades.
Depending on the degree of prolapse, internal hemorrhoids are classified into four grades.
- External hemorrhoids: External hemorrhoids develop due to excessive dilation of the venous plexus below the dentate line and are located beneath the skin surrounding the anal opening.
 Recognizing the Signs of Hemorrhoids
Recognizing the Signs of Hemorrhoids
- Mixed hemorrhoids: Mixed hemorrhoids occur when internal and external hemorrhoids coexist. This condition usually results from weakening and loss of elasticity of the Parks ligament—a structure responsible for keeping internal and external hemorrhoids separate. When the Parks ligament undergoes mucoid degeneration, it can no longer adequately support the hemorrhoidal cushions in their original positions, leading to the development of mixed hemorrhoids.
Risk Factors for Hemorrhoids
- Unhealthy dietary habits
Low fiber intake: A lack of dietary fiber leads to hard stools, causing constipation and increasing pressure on the hemorrhoidal veins.
Consumption of spicy foods: Spicy foods can irritate the anal mucosa, increasing the risk of inflammation.
Insufficient water intake: When the body is dehydrated, stools become dry and hard, making bowel movements difficult and placing additional strain on the hemorrhoidal veins.
- Sedentary lifestyle
Prolonged sitting: Sitting for long periods increases pressure on the hemorrhoidal veins, especially among office workers.
Lack of physical activity: Physical inactivity slows digestion and increases the risk of constipation.
 Risk Factors for Hemorrhoids
Risk Factors for Hemorrhoids
-
Obesity
Increased intra-abdominal pressure: Obesity increases pressure on the veins, leading to dilation of the hemorrhoidal veins.
Metabolic disorders: Obesity is often associated with metabolic abnormalities, which increase the risk of various conditions, including hemorrhoids.
-
Pregnancy and childbirth
Increased abdominal pressure: As the fetus grows, pressure on the pelvic veins increases, causing dilation of the hemorrhoidal veins.
Straining during labor: Forceful pushing during childbirth is also a significant risk factor.
-
Other factors
Chronic diarrhea: Causes irritation of the anal mucosa, increasing the risk of inflammation.
Alcohol consumption: Increases portal venous pressure, contributing to dilation of hemorrhoidal veins.
Underlying medical conditions: Conditions such as liver cirrhosis and heart failure may also increase the risk of developing hemorrhoids.
Occupational factors: Jobs that involve heavy physical labor (e.g., manual handlers, weightlifters, tennis players) or prolonged standing or sitting (e.g., secretaries, tailors, sales staff).
Abnormal pelvic masses: Including colorectal tumors and uterine tumors.
Symptoms of Hemorrhoids
The symptoms of hemorrhoids may vary depending on the type and grade of the condition. Internal hemorrhoids usually do not cause pain but may lead to bleeding during bowel movements and a feeling of fullness or pressure in the anal area. As the disease progresses, the hemorrhoidal cushions may prolapse outside the anus.
External hemorrhoids often cause pain, itching, and swelling, and the hemorrhoids may be visibly noticeable on the skin around the anal opening. Both types of hemorrhoids can cause discomfort and negatively affect quality of life.
 Pain, Itching, and Anal Swelling as Signs of Hemorrhoids
Pain, Itching, and Anal Swelling as Signs of Hemorrhoids
Common symptoms used to recognize hemorrhoids include:
-
Rectal bleeding during bowel movements: This is a common symptom and often the main reason patients seek medical care. The blood is typically bright red and may drip or spurt in a stream, similar to “chicken bloodletting.”
-
Prolapse of hemorrhoids outside the anal canal: This may occur during bowel movements, walking, or prolonged squatting. Initially, the hemorrhoids may retract spontaneously; later, manual reduction is required, and eventually they may remain prolapsed continuously.
-
Itching or irritation in the anal area: This is caused by mucus discharge from the lining of the anal canal.
-
Pain or discomfort: Pain may range from mild to severe due to thrombosed hemorrhoids (formation of blood clots within the hemorrhoidal cushions), strangulated prolapsed hemorrhoids leading to swelling and edema, or associated anal fissures, which can cause severe pain during defecation.
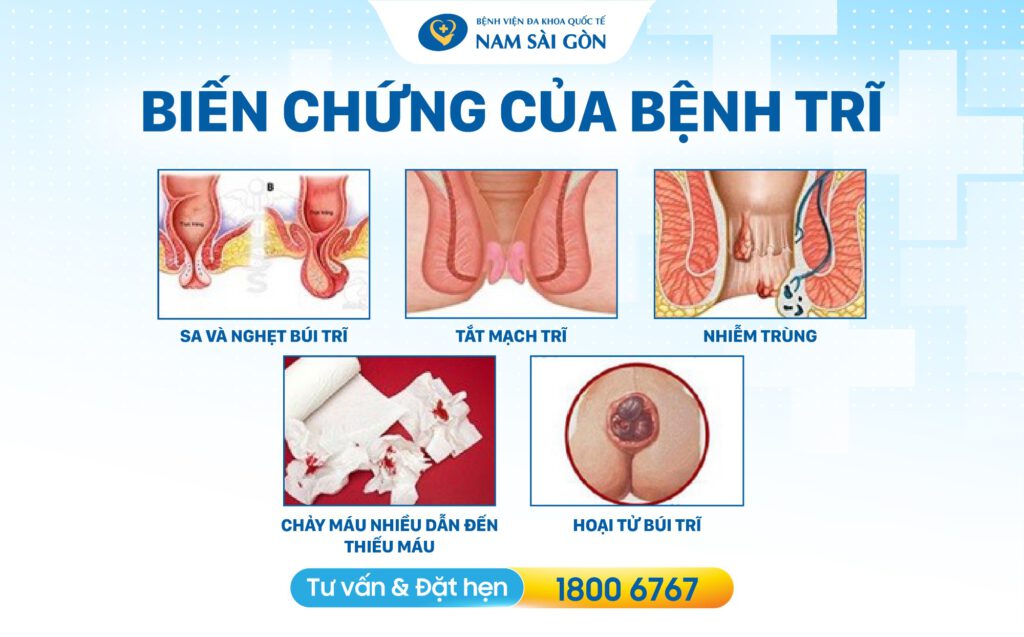
Complications of Hemorrhoids
Serious complications of hemorrhoids include:
-
Heavy bleeding leading to anemia
Cause: Hemorrhoidal cushions may be injured during bowel movements, resulting in frequent bleeding, which can lead to chronic anemia or a reduction in red blood cell indices.
Symptoms: Bright red blood on toilet paper, blood mixed with stool, or blood spurting in a stream.
Consequences: Anemia, fatigue, dizziness, and in severe cases, profound anemia.
-
Infection
Cause: Bacteria can enter open wounds on hemorrhoids, causing inflammation and possible infection of the perianal skin.
Symptoms: Anal pain and burning sensation, swelling, fever, and purulent discharge.
Consequences: The infection may spread, leading to perianal abscesses or even sepsis.
-
Thrombosed hemorrhoids
Cause: Blood clots form within the hemorrhoidal cushions, leading to vascular obstruction. Factors such as forceful straining, heavy lifting, pregnancy, or prolonged sitting increase the risk of thrombosis.
Symptoms: Marked swelling of the hemorrhoids, severe pain, and a bluish or purplish discoloration.
Consequences: If not treated promptly, the hemorrhoids may become necrotic.
 Hemorrhoids Can Lead to Serious Complications
Hemorrhoids Can Lead to Serious Complications
-
Prolapse and strangulation of hemorrhoids
Cause: The hemorrhoidal cushions prolapse outside the anus and are unable to retract spontaneously. Strangulation may occur, leading to obstruction of blood vessels.
Symptoms: Severe pain; markedly swollen, tense, and reddened hemorrhoids; inability to manually reduce the prolapse; difficulty walking. In some cases, black spots may appear on the strangulated hemorrhoids, indicating tissue necrosis.
Consequences: Strangulated hemorrhoids can result in tissue necrosis and infection.
-
Hemorrhoidal necrosis
Cause: Caused by thrombosis, infection, or trauma.
Symptoms: The necrotic hemorrhoidal tissue turns black due to irreversible tissue damage and progressive cell death, often accompanied by a foul odor.
Consequences: Severe pain and serious infection, which may become life-threatening if not treated promptly.
-
Rectal cancer (rare)
Cause: Chronic inflammation in the anorectal region may increase the risk of cancer.
Symptoms: Changes in bowel habits, blood in the stool, and unexplained weight loss.
Diagnosis of Hemorrhoids
To diagnose hemorrhoids, physicians perform a thorough anorectal examination, including a digital rectal examination and proctoscopy. Additional laboratory tests, such as blood tests, may also be ordered. These evaluations allow the physician to accurately determine the type of hemorrhoids, assess disease severity, and develop an appropriate treatment plan.
Digital rectal examination
This is a mandatory step in anorectal examinations in general and in the diagnosis of hemorrhoids in particular. The purpose of a digital rectal examination is not only to diagnose hemorrhoids but also to avoid missing other conditions in which hemorrhoids may be only a symptom, such as rectal cancer, and to preliminarily assess anal sphincter tone.
The patient is asked to remove clothing from the waist down and change into a hospital gown. The physician wears gloves, applies a lubricant, and gently inserts a finger into the rectum to examine and identify any abnormal changes within the anal canal.
Blood tests
-
Purpose: To assess the degree of anemia caused by excessive rectal bleeding.
-
Findings: Blood test results help the physician evaluate the presence and severity of hemorrhoids. Additionally, an elevated white blood cell count may indicate an anal infection—a common complication associated with hemorrhoids.
Defecography using video proctoscopy (Video proctoscope)
In the past, diagnosis relied mainly on patient-reported symptoms to estimate the degree of internal hemorrhoid prolapse. With advances in technology, video recording systems installed in restroom settings now allow real-time visualization of the defecation process. This modern method helps accurately determine the degree of internal hemorrhoid prolapse and identify other anorectal disorders.
 Defecation Imaging Method (Video Proctoscope)
Defecation Imaging Method (Video Proctoscope)
Anorectal Endoscopy (Proctoscopy)
After the clinical examination, patients may be advised by the physician to undergo rectal endoscopy. Through the endoscope, hemorrhoidal cushions can be clearly visualized as bulging areas of mucosa with a darker color, typically located at the 4 o’clock, 7 o’clock, and 11 o’clock positions. Anorectal endoscopy is considered the most effective and valuable method for diagnosing Grade I internal hemorrhoids.
In addition, this procedure helps detect other anorectal lesions such as anal fissures, anorectal polyps, rectal cancer, and anal canal cancer—which are often mistaken for hemorrhoids due to similar symptoms such as rectal bleeding—as well as rectal prolapse. Although rectal prolapse is relatively uncommon, the prolapsed mass appears at the anus during defecation and has characteristics that are distinctly different from prolapsed hemorrhoids.
A rectal prolapse typically has a regular shape and is covered with bright pink mucosa. The protruding mass displays concentric circular mucosal folds, with the center of the circles corresponding to the anal opening.
Rectal endoscopy offers several significant advantages, including clear imaging, a minimally invasive approach, minimal discomfort, and the ability to detect diseases at an early stage. Compared with traditional anorectal examination methods, rectal endoscopy represents a major advancement in diagnostic imaging.
Rectal endoscopy is indicated for patients presenting with symptoms such as rectal bleeding, anal pain or burning sensation, prolapsed hemorrhoids, or when other anorectal diseases are suspected.

Treatment of Hemorrhoids
Principles of Treatment
Hemorrhoids should not be treated solely based on symptoms unless complications are present.
(Symptomatic hemorrhoids refer to hemorrhoids that develop due to specific and identifiable causes such as late-stage pregnancy, rectal cancer, uterine cancer, or pelvic and perineal tumors that compress venous return, leading to engorgement of the hemorrhoidal plexus and formation of hemorrhoids.)
Treatment is indicated only when hemorrhoids cause disturbances that affect quality of life, work performance, or overall health.
Before initiating hemorrhoid treatment, underlying conditions considered to be contributing factors must be addressed. Hemorrhoids present with various types of lesions and degrees of severity; therefore, treatment should be selected based on the specific characteristics and extent of the disease.
Prevention and management of contributing factors
Dietary management
-
Consume plenty of vegetables such as spinach, kale, Malabar spinach, sweet potato leaves, and amaranth
-
Increase fruit intake
-
Drink adequate amounts of water
-
Limit alcohol, beer, tobacco, coffee, and strong tea
-
If constipation is present, laxatives may be used intermittently but should not be taken for prolonged periods
Lifestyle modifications
-
Avoid prolonged sitting
-
Establish regular bowel habits
-
Avoid staying up late
-
Engage in regular physical exercise and moderate sports activities
Work-related considerations
- Avoid excessive heavy labor
- Avoid sudden forceful movements that abruptly increase intra-abdominal pressure
Management of bowel disorders
If conditions such as chronic colitis or irritable bowel syndrome are present, they should be treated prior to hemorrhoid management.
Management of existing chronic diseases
Chronic conditions such as bronchitis, hypertension, diabetes, and benign prostatic hyperplasia causing urinary retention should also be treated concurrently.
Medical (Conservative) Treatment
Medical treatment includes the use of medications with the following effects: strengthening the venous walls (e.g., Daflon, Ginkor Fort), relieving pain and itching (menthol, cocaine derivatives), reducing edema (alpha-chymotrypsin, warm sitz baths), and preventing or treating infection (antibiotics).
Conservative treatment is effective only for Grade I and Grade II hemorrhoids. Patients should undergo proper medical examination and follow the physician’s instructions; self-treatment at home is not recommended.
Minimally Invasive Procedures
Sclerotherapy (Injection therapy)
This method is based on inducing shrinkage and fibrosis of the hemorrhoidal cushions by injecting a sclerosing agent directly into the hemorrhoids. It is particularly effective for early-stage hemorrhoids, especially Grade I and Grade II.
Infrared coagulation
This is a minimally invasive treatment that uses infrared radiation to coagulate the hemorrhoidal tissue. The infrared energy generates heat that coagulates the blood vessels supplying the hemorrhoids. Once the blood supply is interrupted, the hemorrhoids gradually shrink and slough off. This method is indicated for small hemorrhoids that are not suitable for rubber band ligation.
Rubber band ligation
This is a commonly used method for treating internal hemorrhoids. It is simple to perform, cost-effective, and can be done on an outpatient basis. Rubber band ligation is ideal for Grade II and Grade III internal hemorrhoids.
Surgical Treatment
Surgery is indicated when conservative treatment fails, in cases of Grade III–IV hemorrhoids, thrombosed hemorrhoids, circumferential prolapsed hemorrhoids, or severe hemorrhagic hemorrhoids.
Currently, two surgical techniques are commonly used for hemorrhoidectomy: the conventional hemorrhoidectomy (Milligan–Morgan procedure) and the Longo procedure. Among these, the Longo procedure—currently applied at Nam Sai Gon International General Hospital—is considered a minimally painful, effective, and time-efficient method, typically completed within approximately 30 minutes.
Conventional Hemorrhoidectomy (Milligan–Morgan Procedure)
Principle:
Each hemorrhoidal cushion is excised individually. Between the excised hemorrhoids, segments of skin and mucosa are preserved. These segments—referred to as mucocutaneous bridges—consist of skin externally and mucosa internally, and help prevent postoperative anal stenosis.
Advantages:
-
Relatively less postoperative pain
-
Widely used in current clinical practice
Disadvantages:
-
Excess residual skin and mucosa may remain, which can cause psychological discomfort for some patients

Longo Procedure (Stapled Hemorrhoidopexy) The Longo procedure, currently applied at Nam Sai Gon International General Hospital, is considered a minimally painful, effective, and time-efficient treatment for hemorrhoids, typically completed within approximately 30 minutes.
Longo procedure (stapled hemorrhoidopexy):
Principle:
This technique involves excising and stapling the prolapsed rectal mucosa in patients with Grade II, III, and IV hemorrhoids, including circumferential hemorrhoids, using a circular stapling device. The resection and stapling line is located above the dentate line.
Advantages:
-
Minimal to no postoperative pain
-
Early discharge and rapid recovery
Disadvantages:
-
Technically challenging in cases of mixed hemorrhoids with excessive external skin
-
Higher cost
-
Higher rates of postoperative complications such as bleeding and anal stenosis compared with conventional hemorrhoidectomy
Prevention of Hemorrhoids
-
Increase dietary fiber intake in daily meals and include foods and beverages that support digestive health, such as drinking water, fresh fruit juices, yogurt, green leafy vegetables, root vegetables, and mushrooms.
-
Limit the consumption of alcohol, beer, coffee, spicy foods, and heavily seasoned dishes.
-
Establish regular bowel habits and avoid excessive straining during defecation. If chronic constipation is present, the use of laxatives and stool softeners may help reduce pressure during bowel movements.
-
Engage in physical exercise for 15–30 minutes per day to improve bowel motility, reduce the risk of constipation, and prevent recurrence of hemorrhoids.
-
Avoid prolonged sitting. For office workers, it is recommended to stand up and walk around after every 2 hours of work.
-
Limit late nights, stress, and psychological pressure.
-
Warm saltwater sitz baths may be used to soften the perianal skin and reduce pressure during bowel movements.

Internal and external hemorrhoids significantly affect health and quality of life. Moreover, if not managed promptly, the condition may worsen and lead to serious complications. Therefore, patients are advised to seek early medical consultation and follow treatment recommendations from specialist physicians.
Nam Sai Gon International General Hospital accepts National Health Insurance and Private Health Insurance, providing convenient and comprehensive care for patients.
Nam Sai Gon International General Hospital
No. 88, Street No. 8, Trung Son Residential Area, Binh Hung Commune, Ho Chi Minh City.
Hotline: 18006767
info@nih.com.vn
Last updated: 10:42 17/01/2026
- https://vi.wikipedia.org/wiki/Tr%C4%A9_(b%E1%BB%87nh)
- https://www.mayoclinic.org/diseases-conditions/hemorrhoids/symptoms-causes/syc-20360268
- https://www.healthline.com/health/hemorrhoids#What-are-hemorrhoids
- https://www.webmd.com/digestive-disorders/understanding-hemorrhoids-basics
- https://www.medicalnewstoday.com/articles/73938#treatment






